-
OK, it's on.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
What do you guys score on this test?
- Thread starter Nofriends
- Start date
Nebulous
Well-Known Member
Paranoid |||||||||||||||| 69% 50%
Schizoid |||||||||||||| 52% 40%
Schizotypal |||||||||||||||||||| 84% 56%
Antisocial |||||||||||||||||| 78% 46%
Borderline |||||||||||||||||| 73% 45%
Histrionic |||||||||||||| 60% 52%
Narcissistic |||||||||||||| 52% 40%
Avoidant |||||||||||||||||| 78% 48%
Dependent |||||||||||||||| 68% 44%
OCD |||||| 27% 45%
This test really wasn't done that well tbh.
If you're interested in self diagnosing yourself with something, don't rely on results from quizzes like this.
I've been diagnosed with OCD and it was the lowest score I got on this test.
Schizoid |||||||||||||| 52% 40%
Schizotypal |||||||||||||||||||| 84% 56%
Antisocial |||||||||||||||||| 78% 46%
Borderline |||||||||||||||||| 73% 45%
Histrionic |||||||||||||| 60% 52%
Narcissistic |||||||||||||| 52% 40%
Avoidant |||||||||||||||||| 78% 48%
Dependent |||||||||||||||| 68% 44%
OCD |||||| 27% 45%
This test really wasn't done that well tbh.
If you're interested in self diagnosing yourself with something, don't rely on results from quizzes like this.
I've been diagnosed with OCD and it was the lowest score I got on this test.
Nofriends
Banned
I am 1% more narcissistic than you hahaha
Happy
sorry for english
Paranoid 42%
Schizoid 51%
Schizotypal 76%
Antisocial 65%
Borderline 50%
Histrionic 45%
Narcissistic 62%
Avoidant 34%
Dependent 35%
Obsessive-Compulsive 53%
Haha so I'm apparently a schizotypal, antisocial narcissist. Doesn't sound like me at all!
Schizoid 51%
Schizotypal 76%
Antisocial 65%
Borderline 50%
Histrionic 45%
Narcissistic 62%
Avoidant 34%
Dependent 35%
Obsessive-Compulsive 53%
Haha so I'm apparently a schizotypal, antisocial narcissist. Doesn't sound like me at all!
Sinny91
Banned
Paranoid |||||||||||||||| 65% 50%
Schizoid |||||||||||||| 56% 40%
Schizotypal |||||||||||||||||||| 86% 56%
Antisocial |||||||||||||||| 67% 46%
Borderline |||||||||||||||| 67% 45%
Histrionic |||||||||||||| 53% 52%
Narcissistic |||||||||||||| 55% 40%
Avoidant |||||||||||||||| 69% 48%
Dependent |||||||||||||||| 62% 44%
Obsessive-Compulsive |||||||||||| 41% 45%
Lol, maybe I have been crazy this whole time...
http://www.youtube.com/watch?v=i4v-yvf2ELI
Schizoid |||||||||||||| 56% 40%
Schizotypal |||||||||||||||||||| 86% 56%
Antisocial |||||||||||||||| 67% 46%
Borderline |||||||||||||||| 67% 45%
Histrionic |||||||||||||| 53% 52%
Narcissistic |||||||||||||| 55% 40%
Avoidant |||||||||||||||| 69% 48%
Dependent |||||||||||||||| 62% 44%
Obsessive-Compulsive |||||||||||| 41% 45%
Schizotypal personality disorder (STPD) or schizotypal disorder is a mental disorder characterized by severe social anxiety, paranoia, and often unconventional beliefs. People with this disorder feel extreme discomfort with maintaining close relationships with people, mainly for the fact that they think that their peers harbor negative thoughts towards them, so they avoid forming them. Peculiar speech mannerisms and odd modes of dress are also diagnostic signs of this disorder. In some cases, people with STPD may react oddly in conversations, not respond, or talk to themselves.[1]
They frequently misinterpret situations as being strange or having unusual meaning for them; paranormal and superstitious beliefs are common. Such people frequently seek medical attention for anxiety or depression instead of their personality disorder.[2] Schizotypal personality disorder occurs in approximately 3% of the general population and is slightly more common in males.
Lol, maybe I have been crazy this whole time...
http://www.youtube.com/watch?v=i4v-yvf2ELI
https://en.wikipedia.org/wiki/Schizotypal_personality_disorderIn most instances, schizotypal personality disorders co-occurs with the schizoid, paranoid, avoidant, and borderline personality disorders
Diagnosis
DSM-5
In the American Psychiatric Association's DSM-5, schizotypal personality disorder is defined as a "pervasive pattern of social and interpersonal deficits marked by acute discomfort with, and reduced capacity for, close relationships as well as by cognitive or perceptual distortions and eccentricities of behavior, beginning by early adulthood and present in a variety of contexts."[19]
At least five of the following symptoms must be present: ideas of reference, strange beliefs or magical thinking, abnormal perceptual experiences, strange thinking and speech, paranoia, inappropriate or constricted affect, strange behavior or appearance, lack of close friends, and excessive social anxiety that does not abate and stems from paranoia rather than negative judgments about self. These symptoms must not occur only during the course of a disorder with similar symptoms (such as schizophrenia or autism spectrum disorder).[19]
(I call sane, I think I only qualify for 4 and a half of those)
A disorder characterized by eccentric behavior and anomalies of thinking and affect which resemble those seen in schizophrenia, though no definite and characteristic schizophrenic anomalies have occurred at any stage.
There is no dominant or typical disturbance, but any of the following may be present:
Inappropriate or constricted affect (the individual appears cold and aloof);
Behavior or appearance that is odd, eccentric or peculiar;
Poor rapport with others and a tendency to withdraw socially;
Odd beliefs or magical thinking, influencing behavior and inconsistent with subcultural norms;
Suspiciousness or paranoid ideas;
Obsessive ruminations without inner resistance, often with dysmorphophobic, sexual or aggressive contents;
Unusual perceptual experiences including somatosensory (bodily) or other illusions, depersonalization or derealization;
Vague, circumstantial, metaphorical, over-elaborate or stereotyped thinking, manifested by odd speech or in other ways, without gross incoherence;
Occasional transient quasi-psychotic episodes with intense illusions, auditory or other hallucinations and delusion-like ideas, usually occurring without external provocation.
The disorder runs a chronic course with fluctuations of intensity. Occasionally it evolves into overt schizophrenia. There is no definite onset and its evolution and course are usually those of a personality disorder. It is more common in individuals related to people with schizophrenia and is believed to be part of the genetic "spectrum" of schizophrenia.
Therapy
According to Theodore Millon, the schizotypal is one of the easiest personality disorders to identify but one of the most difficult to treat with psychotherapy.[21][page needed] Persons with STPD usually consider themselves to be simply eccentric, creative, or nonconformist. As a rule, they underestimate maladaptiveness of their social isolation and perceptual distortions. It is not so easy to develop rapport with people who suffer from STPD due to the fact that increasing familiarity and intimacy usually increase their level of anxiety and discomfort. In most cases they do not respond to informality and humor
peoplesuck
is escaping
QuickTwist
Spiritual "Woo"
I usually just post an image of the results I got with no in depth analysis if I thought the test was mediocre, but this test is one of the worst I have seen. I cannot take a test seriously that asks "I think its important that people think I'm awesome." That is beyond humorous to me.
deathvirtuoso
Active Member
- Local time
- Today 7:36 AM
- Joined
- Mar 30, 2016
- Messages
- 112
Paranoid |||||||||||||| 53% 50%
Schizoid |||||||||||| 41% 40%
Schizotypal |||||||||||||||||||| 85% 56%
Antisocial |||||||||||||||||||| 82% 46%
Borderline |||||||||||||||| 65% 45%
Histrionic |||||||||||| 50% 52%
Narcissistic |||||||||||||| 54% 40%
Avoidant |||||||||||||| 58% 48%
Dependent |||||||||||| 50% 44%
Obsessive-Compulsive |||| 18% 45%
As nebulous has said, the test wasn't done well. I couldn't really take this test very seriously, and I was really distracted when I did the test, so I wouldn't really care too much about my results. (Man, I tend to overuse 'really')
Schizoid |||||||||||| 41% 40%
Schizotypal |||||||||||||||||||| 85% 56%
Antisocial |||||||||||||||||||| 82% 46%
Borderline |||||||||||||||| 65% 45%
Histrionic |||||||||||| 50% 52%
Narcissistic |||||||||||||| 54% 40%
Avoidant |||||||||||||| 58% 48%
Dependent |||||||||||| 50% 44%
Obsessive-Compulsive |||| 18% 45%
As nebulous has said, the test wasn't done well. I couldn't really take this test very seriously, and I was really distracted when I did the test, so I wouldn't really care too much about my results. (Man, I tend to overuse 'really')
onesteptwostep
Junior Hegelian
- Local time
- Today 8:36 AM
- Joined
- Dec 7, 2014
- Messages
- 4,251
Paranoid |||||||||||| 47% 50%
Schizoid |||||||||||| 46% 40%
Schizotypal |||||||||||||| 57% 56%
Antisocial |||||||||||| 50% 46%
Borderline |||||||||||| 49% 45%
Histrionic |||||||||||| 45% 52%
Narcissistic |||||||||||||| 51% 40%
Avoidant |||||||||||| 45% 48%
Dependent |||||||||||| 45% 44%
Obsessive-Compulsive |||||||||||| 46% 45%
The highest deviation from the average are narcissism and histronicsm (7~9%ish), other than that the results pretty mellow.
Schizoid |||||||||||| 46% 40%
Schizotypal |||||||||||||| 57% 56%
Antisocial |||||||||||| 50% 46%
Borderline |||||||||||| 49% 45%
Histrionic |||||||||||| 45% 52%
Narcissistic |||||||||||||| 51% 40%
Avoidant |||||||||||| 45% 48%
Dependent |||||||||||| 45% 44%
Obsessive-Compulsive |||||||||||| 46% 45%
The highest deviation from the average are narcissism and histronicsm (7~9%ish), other than that the results pretty mellow.
marie
Member
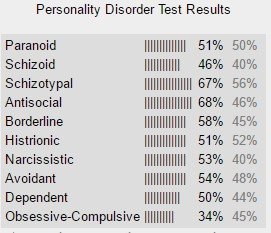
Paranoid |||||||||||||| 51% 50%
Schizoid |||||||||||||| 57% 40%
Schizotypal |||||||||||||| 56% 56%
Antisocial |||||||||||| 48% 46%
Borderline |||||||||||||| 54% 45%
Histrionic |||||||||||||||||| 73% 52%
Narcissistic |||||||||||||||||| 75% 40%
Avoidant |||||||||| 40% 48%
Dependent |||||||||||| 48% 44%
Obsessive-Compulsive |||||||||||||||||| 78% 45%
Schizoid |||||||||||||| 57% 40%
Schizotypal |||||||||||||| 56% 56%
Antisocial |||||||||||| 48% 46%
Borderline |||||||||||||| 54% 45%
Histrionic |||||||||||||||||| 73% 52%
Narcissistic |||||||||||||||||| 75% 40%
Avoidant |||||||||| 40% 48%
Dependent |||||||||||| 48% 44%
Obsessive-Compulsive |||||||||||||||||| 78% 45%
Paranoid |||||| 30% 50%
Schizoid |||||||||||||||| 62% 40%
Schizotypal |||||||||||||||| 70% 56%
Antisocial |||||||||| 38% 46%
Borderline |||||| 26% 45%
Histrionic |||||||||||| 46% 35%
Narcissistic |||||||||||| 42% 40%
Avoidant |||||||||||||||| 66% 48%
Dependent |||||||||| 38% 44%
Obsessive-Compulsive |||||||||||| 42% 45%
Well gee that's awful high
Schizoid |||||||||||||||| 62% 40%
Schizotypal |||||||||||||||| 70% 56%
Antisocial |||||||||| 38% 46%
Borderline |||||| 26% 45%
Histrionic |||||||||||| 46% 35%
Narcissistic |||||||||||| 42% 40%
Avoidant |||||||||||||||| 66% 48%
Dependent |||||||||| 38% 44%
Obsessive-Compulsive |||||||||||| 42% 45%
Well gee that's awful high
AndyC
Hm?
- Local time
- Today 9:36 AM
- Joined
- Nov 30, 2015
- Messages
- 353
Paranoid |||||||||||||| 52% 50%
Schizoid |||||||||||| 44% 40%
Schizotypal |||||||||||||||||||| 85% 56%
Antisocial |||||||||||||||||||| 83% 46%
Borderline |||||||||||||||| 61% 45%
Histrionic |||||||||| 31% 52%
Narcissistic |||||||||| 39% 40%
Avoidant |||||||||||||||| 63% 48%
Dependent |||||||||||| 50% 44%
Obsessive-Compulsive || 9% 45%
*scores in gray are the average web score
Schizoid |||||||||||| 44% 40%
Schizotypal |||||||||||||||||||| 85% 56%
Antisocial |||||||||||||||||||| 83% 46%
Borderline |||||||||||||||| 61% 45%
Histrionic |||||||||| 31% 52%
Narcissistic |||||||||| 39% 40%
Avoidant |||||||||||||||| 63% 48%
Dependent |||||||||||| 50% 44%
Obsessive-Compulsive || 9% 45%
*scores in gray are the average web score
Schizotypal: "preoccupied with seeing themselves and/or the world as strange/odd".
That's just sanity!
Paranoid |||||||||||||| 52% 50%
Schizoid |||||||||||||| 55% 40%
Schizotypal |||||||||||||| 70% 56%
Antisocial |||||||||||||| 60% 46%
Borderline |||||||||||| 50% 45%
Histrionic |||||||||| 33% 52%
Narcissistic |||||||||| 36% 40%
Avoidant |||||||||||||| 59% 48%
Dependent |||||||||||||| 51% 44%
Obsessive-Compulsive |||||||||| 36% 45%
Surprised at how high schizoid is though, although I have been doing a lot of work lately and have been under a great deal of stress, the lack of emotional tuning may just be due to mental fatigue.
The 'Dependent' one is just embarrassing! I couldn't have left my parents house sooner! Either this test is uncovering parts of my deeper conscious I had no idea about, or it's an anomaly.
That's just sanity!
Paranoid |||||||||||||| 52% 50%
Schizoid |||||||||||||| 55% 40%
Schizotypal |||||||||||||| 70% 56%
Antisocial |||||||||||||| 60% 46%
Borderline |||||||||||| 50% 45%
Histrionic |||||||||| 33% 52%
Narcissistic |||||||||| 36% 40%
Avoidant |||||||||||||| 59% 48%
Dependent |||||||||||||| 51% 44%
Obsessive-Compulsive |||||||||| 36% 45%
Surprised at how high schizoid is though, although I have been doing a lot of work lately and have been under a great deal of stress, the lack of emotional tuning may just be due to mental fatigue.
The 'Dependent' one is just embarrassing! I couldn't have left my parents house sooner! Either this test is uncovering parts of my deeper conscious I had no idea about, or it's an anomaly.
Nebulous
Well-Known Member
Paranoid |||||||||||||||| 62% 50%
Schizoid |||||||||||| 48% 40%
Schizotypal |||||||||||||||||| 73% 56%
Antisocial |||||||||||||| 59% 46%
Borderline |||||||||||||||| 65% 45%
Histrionic |||||||||||||| 58% 52%
Narcissistic |||||||||||||| 56% 40%
Avoidant |||||||||||||||| 65% 48%
Dependent |||||||||||||||| 61% 44%
Obsessive-Compulsive |||||||||| 40% 45%
Retake^
And comparison:
I got fucking healthier
Which is cool because I actually have, thanks to therapy and stuff
Schizoid |||||||||||| 48% 40%
Schizotypal |||||||||||||||||| 73% 56%
Antisocial |||||||||||||| 59% 46%
Borderline |||||||||||||||| 65% 45%
Histrionic |||||||||||||| 58% 52%
Narcissistic |||||||||||||| 56% 40%
Avoidant |||||||||||||||| 65% 48%
Dependent |||||||||||||||| 61% 44%
Obsessive-Compulsive |||||||||| 40% 45%
Retake^
And comparison:
Paranoid |||||||||||||||| 69% 50%
Schizoid |||||||||||||| 52% 40%
Schizotypal |||||||||||||||||||| 84% 56%
Antisocial |||||||||||||||||| 78% 46%
Borderline |||||||||||||||||| 73% 45%
Histrionic |||||||||||||| 60% 52%
Narcissistic |||||||||||||| 52% 40%
Avoidant |||||||||||||||||| 78% 48%
Dependent |||||||||||||||| 68% 44%
OCD |||||| 27% 45%
I got fucking healthier
Which is cool because I actually have, thanks to therapy and stuff
Share: